Andrigolitis: Causes, Symptoms, and Treatment Options
Andrigolitis is a relatively rare condition that many people may not be familiar with, yet it can have a significant impact on those who suffer from it. Although not widely discussed in mainstream medical conversations, understanding the symptoms, causes, and available treatments for andrigolitis can help patients and healthcare providers manage the condition more effectively.
This article aims to provide a comprehensive overview of andrigolitis, focusing on its definition, possible causes, symptoms, diagnosis, and treatment options, while also offering insights on how to live with this condition. Let’s explore the intricacies of andrigolitis and gain a deeper understanding of its impact on human health.
What is Andrigolitis?
Andrigolitis is an inflammatory condition that affects specific tissues or organs in the body, leading to pain, swelling, and dysfunction. Although it primarily affects men, it can occur in individuals of any gender, and the exact reasons for its onset remain unclear.
Due to its rarity, andrigolitis is often misdiagnosed or overlooked by healthcare professionals, making early detection and treatment challenging. Understanding the condition’s root causes and risk factors is crucial for healthcare practitioners and patients alike to facilitate timely and effective interventions.
Causes of Andrigolitis
1. Genetic Factors
One of the leading theories behind the development of andrigolitis is genetics. A hereditary predisposition may play a significant role in determining an individual’s susceptibility to the condition. Those with a family history of inflammatory disorders or autoimmune diseases are often at a higher risk of developing andrigolitis.
2. Infections
Infections, particularly viral or bacterial, can trigger inflammatory responses in the body, potentially leading to the onset of andrigolitis. Chronic infections may overstimulate the immune system, causing it to attack healthy tissues, which could result in inflammation characteristic of andrigolitis.
3. Autoimmune Reactions
In many cases, andrigolitis is linked to autoimmune reactions, where the body’s immune system mistakenly identifies its tissues as foreign invaders. This misguided immune response leads to inflammation and damage to specific parts of the body, exacerbating symptoms of the condition.
4. Environmental Triggers
Environmental factors such as pollution, exposure to toxins, and prolonged stress may also contribute to the development of andrigolitis. While these triggers do not directly cause the condition, they can weaken the immune system or worsen existing inflammation, leading to flare-ups.
Symptoms of Andrigolitis
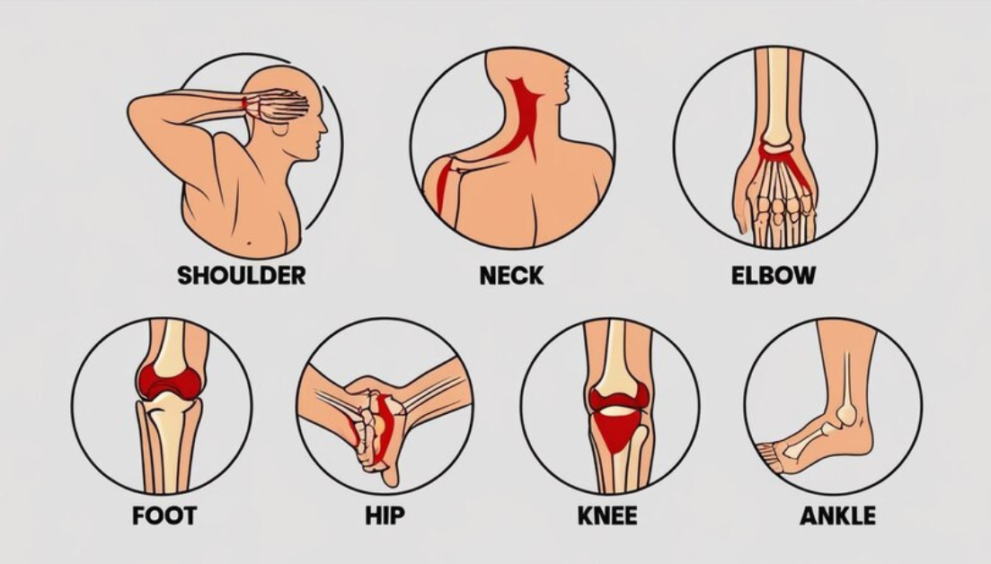
The symptoms of andrigolitis can vary depending on the severity of the inflammation and the areas of the body affected. However, some common signs include:
1. Chronic Pain and Discomfort
Pain is one of the hallmark symptoms of andrigolitis, typically manifesting in the areas of the body where inflammation occurs. This pain can range from mild to severe and may be persistent or come and go in waves.
2. Swelling and Redness
Inflammation often causes visible swelling and redness in the affected areas. The swelling may cause stiffness or reduced mobility, especially if the condition affects joints or muscles.
3. Fever and Fatigue
As with many inflammatory conditions, andrigolitis can lead to fever, chills, and chronic fatigue. The body’s immune system works overtime to combat the inflammation, leaving the individual feeling drained and exhausted.
4. Joint Stiffness and Weakness
If andrigolitis affects the joints, it can lead to significant stiffness and weakness in those areas. Morning stiffness is a common symptom, making movement difficult until the body warms up.
5. Gastrointestinal Issues
In some cases, andrigolitis may also affect the digestive system, causing symptoms like abdominal pain, nausea, or diarrhea. The inflammation may disrupt normal digestion, leading to discomfort and other digestive problems.
Diagnosis of Andrigolitis
Due to its rarity, diagnosing andrigolitis can be challenging. However, early detection is key to preventing long-term damage and managing the condition effectively. A thorough diagnosis typically involves:
1. Medical History and Physical Examination
The first step in diagnosing andrigolitis is obtaining a comprehensive medical history and performing a physical examination. Healthcare providers will ask about any family history of autoimmune or inflammatory conditions and will assess the patient’s symptoms, including the location and duration of the pain or inflammation.
2. Laboratory Tests
Blood tests can be used to measure inflammation levels in the body, typically by assessing markers such as C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR). Elevated levels of these markers may indicate the presence of andrigolitis.
3. Imaging Studies
X-rays, MRIs, or CT scans may be used to evaluate the extent of inflammation and detect any damage to tissues or joints. These imaging tests can provide detailed insights into the severity of the condition and help guide treatment decisions.
4. Biopsy
In some cases, a biopsy may be necessary to confirm the diagnosis. By examining tissue samples under a microscope, healthcare providers can determine the presence of inflammation and other signs indicative of andrigolitis.
Treatment Options for Andrigolitis
While there is no cure for andrigolitis, several treatment options are available to help manage the condition and reduce its impact on daily life. Treatment plans are typically tailored to each individual, depending on the severity of their symptoms and the underlying causes.
1. Medications
a. Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs, such as ibuprofen or naproxen, are often prescribed to reduce inflammation and relieve pain. These medications can be effective in managing mild to moderate cases of andrigolitis.
b. Corticosteroids
In more severe cases, corticosteroids may be prescribed to suppress the immune system and reduce inflammation. While effective, long-term use of these medications can lead to side effects, so they are typically used in short courses.
c. Immunosuppressive Drugs
For patients with autoimmune-related andrigolitis, immunosuppressive drugs may be necessary to manage the condition. These medications help to reduce the immune system’s activity, preventing it from attacking healthy tissues.
d. Biologics
Biologic drugs are a newer class of medications designed to target specific proteins or cells involved in the immune response. These drugs have shown promise in treating autoimmune conditions like andrigolitis, particularly in patients who do not respond well to other treatments.
2. Physical Therapy
Physical therapy is often recommended to help patients manage joint stiffness and improve mobility. Exercises tailored to the patient’s needs can help reduce pain, increase flexibility, and strengthen muscles around the affected areas.
3. Lifestyle Modifications
a. Dietary Changes
Adopting an anti-inflammatory diet can help alleviate some of the symptoms of andrigolitis. Foods rich in omega-3 fatty acids, antioxidants, and vitamins can help reduce inflammation, while processed foods and sugars should be avoided.
b. Stress Management
Since stress can exacerbate inflammation, practicing stress-reducing techniques such as meditation, yoga, or mindfulness can be beneficial for patients with andrigolitis.
c. Exercise
Gentle, low-impact exercises such as swimming, walking, or cycling can help improve circulation, reduce stiffness, and boost overall well-being. Exercise also helps manage weight, which can reduce stress on inflamed joints.
4. Surgical Intervention
In rare and severe cases, surgery may be necessary to repair or replace damaged tissues or joints. Surgery is typically considered a last resort when other treatment options have failed to provide relief.
Living with Andrigolitis
1. Emotional Support
Dealing with a chronic condition like andrigolitis can be emotionally taxing. Seeking support from family, friends, or support groups can provide emotional relief and offer valuable advice from others who understand the condition.
2. Long-Term Management
Since there is no cure for andrigolitis, long-term management is key to improving quality of life. Regular follow-up appointments with healthcare providers, ongoing medication management, and lifestyle adjustments are essential components of living well with the condition.
3. Alternative Therapies
Some patients find relief from alternative therapies such as acupuncture, massage therapy, or herbal supplements. While these therapies should not replace traditional medical treatments, they can complement them and help manage symptoms.
Conclusion
Andrigolitis, though rare, can significantly affect the lives of those who suffer from it. Early diagnosis and proper management are crucial for controlling inflammation, alleviating symptoms, and preventing long-term damage. With a combination of medications, physical therapy, and lifestyle changes, patients can manage their symptoms effectively and improve their overall quality of life.
If you or a loved one is experiencing symptoms consistent with andrigolitis, consult a healthcare professional for an accurate diagnosis and personalized treatment plan. Through informed decision-making and ongoing care, it is possible to live a fulfilling life with andrigolitis.